 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
Take Home Points
Pre-operatively, we review your medical health, present medicines, and allergies
You might need to stop medications that increase bleeding including aspirin
Eye surgeries are done under sedation and pain is minimal
A patch will be on the eye for the first night only
Someone should come with you to the surgicenter
Don’t eat anything after midnight on the day before surgery
One eye is operated on at a time
The surgical options are increasing rapidly
The idea that surgery in an operating room is the last resort has been a frequent comment by patients we care for. In terms of the three main treatments (drops, laser, surgery), the one that could cause vision loss by itself is surgery. This is not very common, but it doesn’t help much to tell a person with a surgical complication that it only happens one in 100 times when they are the one. So, in general, patients do select surgery second or third in line as glaucoma treatments. But, remember that the Collaborative Initial Glaucoma Treatment Study found that surgery before anything else was at least as effective in protecting patients from vision loss as drops. It is the approach most likely to result in no need for daily medication. The decision about which of the three main treatment approaches you want to use was considered in the section What treatments are the right ones? Drops, laser, scissors. Here, we will deal with what patients go through during the various types of glaucoma surgery, why we’d use one over the other one, and what the future holds for promising newer procedures that are being developed.
The traditional types of glaucoma surgery are trabeculectomy, tube-shunt surgery, and diode laser ciliodestruction. At the present time, eye surgeons would most often recommend them in that order, with trabeculectomy being the most commonly performed, especially for those who have not had surgery before. Let’s consider what you’d go through if you choose glaucoma surgery. Many of the events are similar with the 3 surgery types.
Pre-operatively, you would sign an informed consent form after a discussion, in which it is explained that the benefits of surgery are bigger than the risks, and that the risk of surgery is smaller than the risk you now have from the disease as it is being treated. This is a chance to ask questions and make sure that you understand the process. You will have a brief physical exam and review of your medical health and present pills (we need their real names and doses, not just “a blood pressure pill,” so bring along the bottles of medicine). All patients get some form of anesthesia, usually both on the eye itself and through a vein. Typically, there is a nurse anesthetist or an anesthesiologist present who monitors you during the surgery. The eye doctor and the anesthesia staff need to know if you’ve had recent health issues that could affect you during eye surgery. It isn’t that there are big effects on your heart as you might have in abdominal surgery, but the excitement of surgery can run your blood pressure up or get your heart skipping beats. We also need to assure that we don’t give you medicine that you are allergic to, or that would interact badly with your present medicines. We ask you not to eat the morning of surgery, so that in case you get an upset tummy, there’s nothing to bring up.
If it is safe for your overall health, it is particularly important that you stop taking pills that can make you bleed more during eye surgery. These includes aspirin, Coumadin (warfarin), Plavix, Eliquis (and other similar pills), heparin, and any multivitamin that contains vitamin E. Some persons need blood thinners because of serious medical conditions like clots in leg veins, atrial fibrillation heart rhythm, or artificial heart valves. In these cases, we have special ways to keep the blood thinning going and do the surgery anyway. But, if you’re simply taking a baby aspirin or vitamins for good health, stop them as long prior to surgery as possible. Check with your medical doctor first before changing anything.
You’ll have a needle placed in a vein, both to give sedative medicine, and to be able to give you medications in case they’re needed. You will have monitoring devices attached to you for your heart rate, blood pressure (the cuff gets tight), and oxygen level in the blood (on a finger clip). You will be flat on your back in a bed-like stretcher during the surgery, which will take about an hour from coming into the operating room to going back to family. The area around the eye gets prepared in sterile fashion and plastic drapes stick to your face so only the eye is visible to the surgeon. You will not be able to see what is going on during the operation, though quite often you can hear what happens in the room, music, instruments being asked for, and chit chat (to distract you pleasantly).
Before starting, our team gives a medicine through the IV that relaxes you. We numb the area around the eye with a local anesthetic ointment and additional anesthetic under the surface of the eye. For some procedures, we place anesthesia all around the eye by injection while you are sedated. You wake up in a few minutes with no feeling around the eye. An instrument is put in to hold your eye open, so you can’t blink the eye while it is being treated. All you have to do is try to relax and generally keep your body still. If you need to move or cough or scratch your nose, or if you’re in pain, you can just speak up and you will be taken care of by staff. It’s important not to move your arms or legs and not to talk unless there is pain, since all that causes the eye to move. If you get anxious during the surgery, we can give more sedative and narcotics to stop any pain. It is rare, but some extremely anxious patients or others who cannot stay still during surgery elect to have general anesthesia.
The surgeon is looking at your eye through a binocular microscope mounted over the eye and aimed down at you. Also watching are one or more surgical assistants, a nurse handing instruments over, a nurse getting things for us, and anesthesia staff. In a teaching institution like ours, there are large plasma screens with your operation shown to those learning in the room. You will hear the surgeon asking assistants to cut things, hold things, and keep things moist. Believe it or not, we often have four different instruments on or in the eye at one time, so it takes a village.
Unlike general surgery, we never need to do blood transfusions for eye surgery. At the conclusion of surgery, you will most often have a patch placed on the eye to protect it for the first night. The local anesthetic blocks vision as well as feeling, so your vision might be blurry anyway. The eye is much more comfortable patched that first 12 hours. It is tricky getting around with only the unpatched eye—your depth perception is gone, so get help on stairs and curbs. Holding hands with someone friendly is a great idea anytime, but especially now.
It’s mandatory to bring someone with you to the surgicenter the day of surgery. Hospitals have rules that when you get a sedative you shouldn’t go home by yourself. For those having surgery on their better seeing eye, it is obvious that someone will need to help you the night of surgery to do all your essential things, like getting to the bathroom. Overnight admission to the hospital is no longer permitted for standard eye surgery.
For most glaucoma operations, you won’t need much pain medicine. Over the counter pain pills will usually keep you comfortable, but remember: nothing containing aspirin until you are told to restart it. The eye will be sore, especially when you look around, due to some bruising. Eyelids get swollen temporarily, and there can be a black eye as a small amount of blood can seep under the skin of the eyelid. Try to make up a better story for friends than walking into a door. The upper eyelid droops some after most surgeries (called ptosis with a silent “p”). Almost always this goes away by itself—and it keeps you more comfortable by covering the eye more as it heals. If it stays too long, a minor outpatient plastic procedure can be done to raise the lid.
You will almost surely not have the same vision right after surgery as right before, but in most cases vision is back to how it was before surgery within 1-2 weeks. The blurring comes partly from microscopic particles of blood and other tissues inside the eye during this time, and unfortunately, you’re looking through them. Any major worsening of your vision after surgery should be brought to the surgeon’s attention right away.
The operation did something to the surface covering of the eye (conjunctiva), often involving small stitches, so you may have a feeling that something is in the eye. We try to minimize this by making the stitches out of really tiny material and material that absorbs on its own. You’ll be putting in frequent eyedrops as directed by the surgeon, and these help to smooth over the surface. Some of the drops are anti-inflammatory (they help with redness and swelling).
You will be given a set of written instructions with all the detailed “dos and don’ts” that the surgeon suggests. This will deal with physical activity, bathing habits, and travel. Along with this will be the emergency phone number. It is far better to call and ask a question that you think might be silly than to take a chance that you’ll not want to bother the surgeon and let something bad go on too long.
Except in infants, it is very rare for eye surgery to be done in both eyes on the same day.
Take home points for trabeculectomy
It works by producing a controlled leak of eye fluid outward
The area of surgery (bleb) is not usually visible except when you lift your eyelid
The target pressure is reached gradually by releasing stitches, painlessly
Success is achieved for years in the majority of patients
Problem areas are: too low eye pressure, late infection, and cataract
Trabeculectomy means removing a piece of the trabecular meshwork. It followed similar operations done since 1900. Their general purpose is to let water leak from inside the eye, out through the wall of the eye and under the covering tissue (conjunctiva) where it slowly leaks into the tears. Peter Watson of England developed the concept of the present surgery in the 1960s and improvements have been added about every 5 years since then. To summarize what is done (Figure 23), the eye has two layers near the junction of the white and colored part: these are the conjunctiva, a flexible tissue a lot like sandwich wrap, and the sclera, the strong white part of the eye. The surgeon cuts and folds back the conjunctiva, makes an apron-shaped flap half-way down within the sclera, folds the flap back and removes tissue enough to make a hole into the front chamber of the eye. The iris would plug up this hole from the inside, so a piece of iris is removed right under the hole. The flap is put back and sewn in place with tiny nylon sutures that act to keep all the aqueous from running out immediately. Therefore, trabeculectomy is essentially an adjustable valve. Then, the conjunctiva is sewn back in place to cover the area and to begin allowing aqueous to come through it slowly, like a sponge.
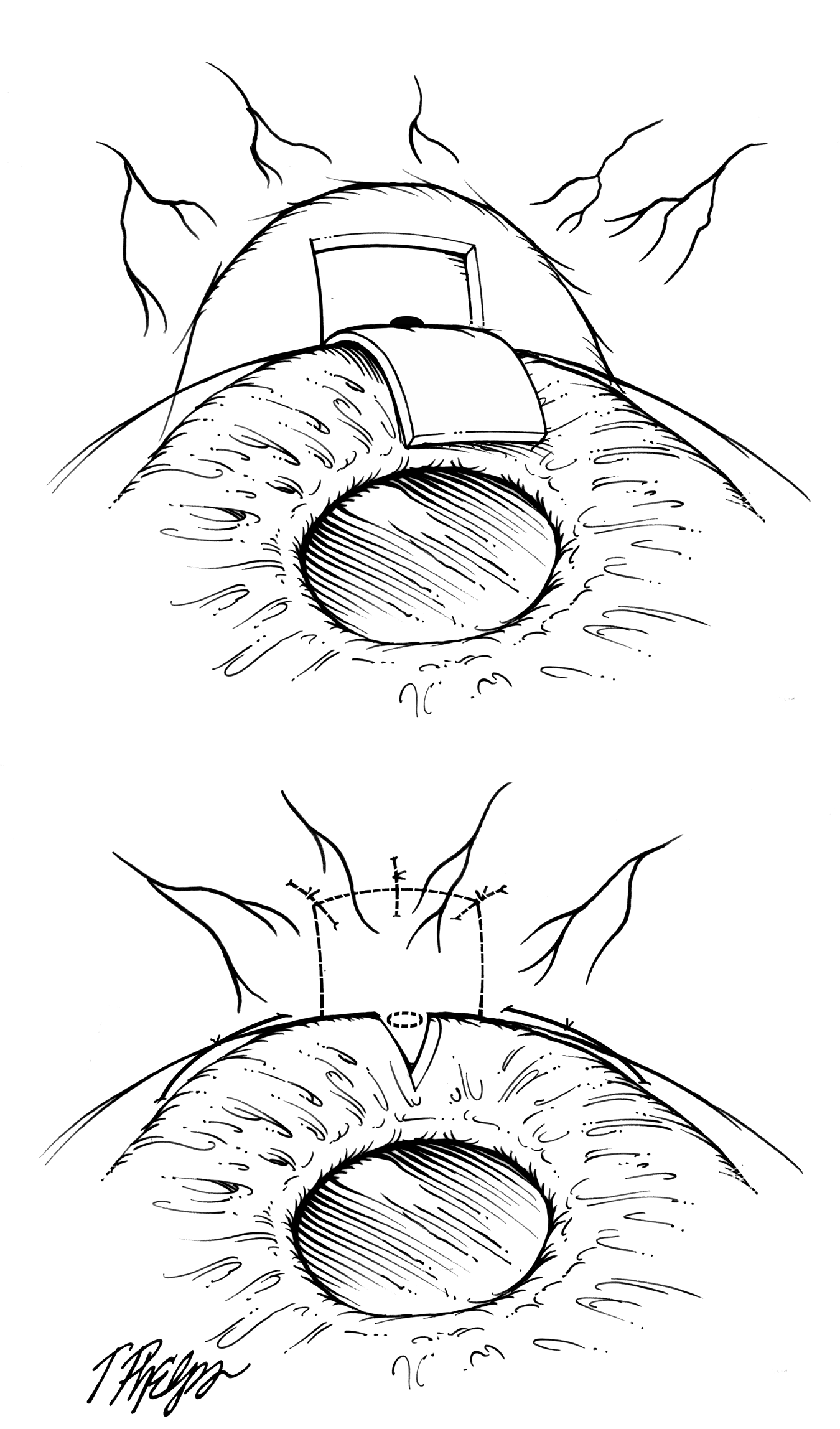 |
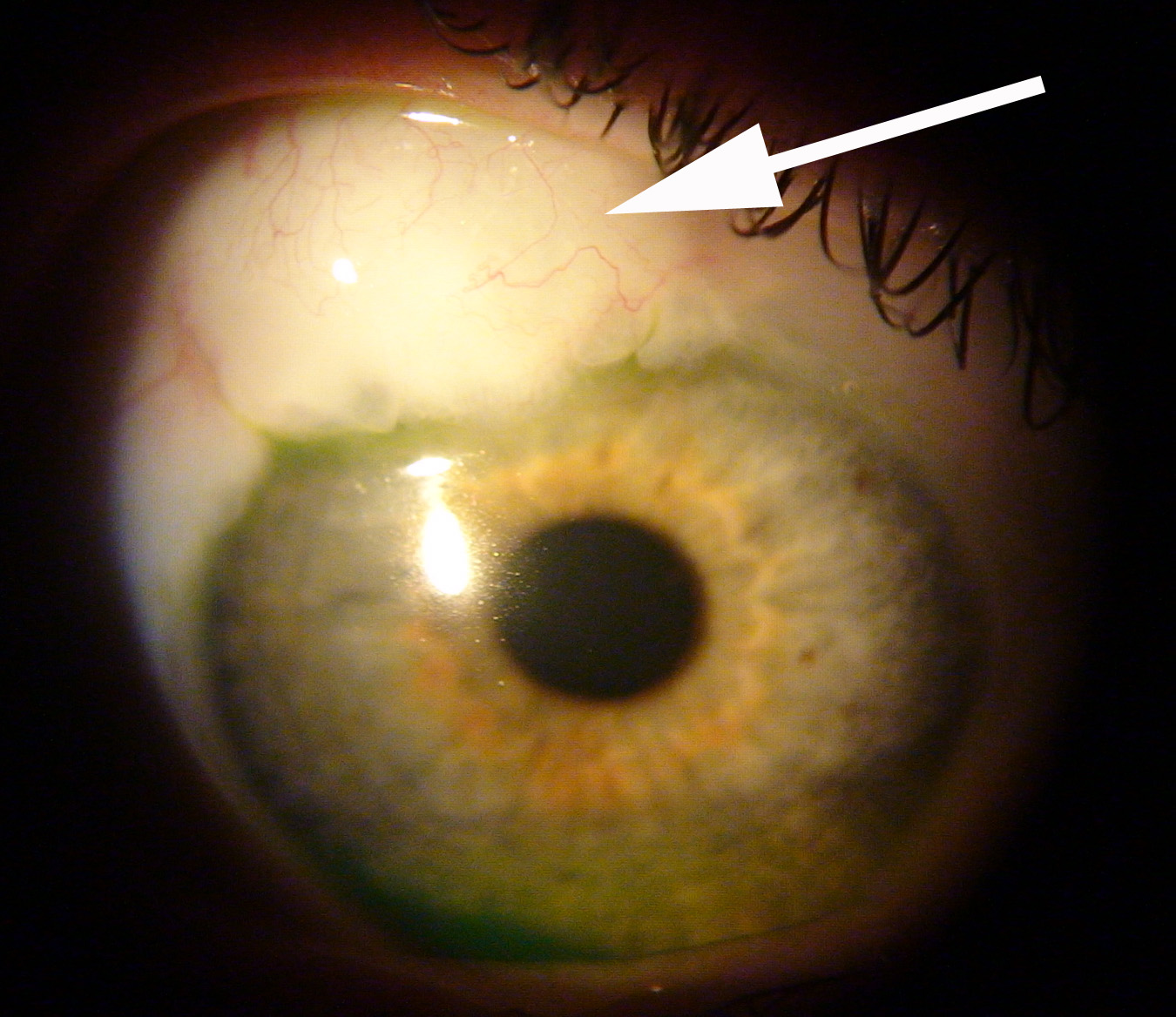
The area of trabeculectomy is always under the upper eyelid – there’s room up there for 2 of them if the first one doesn’t work long enough. Most often others can’t see where it was done, since it’s covered by the eyelid. The surgical area can be elevated somewhat by the fluid coming out. It usually has fewer blood vessels over it than the surrounding conjunctiva, so it looks whiter there. Eye surgeons call this the bleb, since it looks something like a bubble (Figure 24). We tell patients it will be there, but often they forget and six months later they are startled to raise their eyelid and notice the bleb. Mrs. Quigley calls this the "Saturday Morning I Just Noticed My Bleb" emergency call. It’s always good to be able to reassure someone that we call the bleb a success, not a problem.
 |
The trabeculectomy works when more aqueous fluid gets out of the eye and the new pressure is at or below the target (see section What is the target eye pressure?). This means we have to fool the body into thinking it healed the opening shut when it didn’t. Several things help to do this. One is how the flap is constructed. Another is that the eye’s own aqueous fluid actually prevents healing, for the same reason that the iris doesn’t heal shut a laser iridotomy. Third, we often put a strong anti-healing medicine on the eye at the time of surgery to discourage the internal opening from closing—this is the drug mitomycin-C. Finally, you will be putting anti-inflammation eye drops on every few hours for a couple weeks and then slowly decreasing it, which is the final and important step in making the operation work by keeping the hole open.
Early after surgery, we want the pressure to stay a bit over the target. It helps to fool the eye into thinking nothing happened. So, on the one day, one week, and three week visits (there are about four visits all together), you may hear that the pressure is still higher than the target. We plan for that and lower it into the target range gradually. It is important that the pressure doesn’t drop too low too quickly. Remember that the flap of sclera was sewn with stitches—these can be released or melted to reduce their tension, so aqueous flows faster through the hole and the pressure falls. Some surgeons use releasable sutures that are removed during a standard eye exam without any pain. More commonly, they are released painlessly by a tiny laser delivery, one at a time.
We can tell a lot about how the operation is working during the first weeks. A few weeks or months after the operation, you’ll be stopping all eye drops to see if the target is achieved. We have patients whose trabeculectomy is still working 30 years later. Unfortunately, they all don’t work for three decades. About 20% of trabeculectomies fail to control pressure by one year. After that, about one in 25 (4%) stops working each year. In a review of trabeculectomies done at the Wilmer Glaucoma Center of Excellence, with lots of different patients, some with very difficult problems, nearly two-thirds were still at their target and on no medicine five years afterwards, and no further surgery had been needed for the eye.
The main problems that come up after trabeculectomy (other than a failure of the pressure to go down) are: too low a pressure early or later infection, discomfort caused by the bleb area, and bleeding inside the eye. Low pressure can cause blurred or variable vision, and this can happen both with a large hole in the bleb wall or without it. When pressure is very low, the layers of the eye wall can fail to stay in their normal position. They drift off into the eye, causing dark shadows that block vision. These are called choroidal detachments and, while they do not harm the eye permanently, they require treatment often to restore normal position. Another condition can occur when the pressure is low is called hypotony maculopathy. In this, the back of the eye becomes slightly folded (like a balloon losing air), blurring vision. While these are uncommon events, they can lead to permanent changes in vision. Dysfunctionally low pressure (hypotony) is fixed by removing the conjunctiva over the bleb, advancing the conjunctiva to cover the area, and restitching the flap back tightly. This is most often successful and in the vast majority, vision is improved and the target pressure is still achieved.
Any operation can have bacteria enter the eye during surgery. These are most often the patient’s own bacteria that normally live on the eye’s surface. We take steps to keep them out of the eye and to sterilize the eye surface just prior to and during surgery, but one in 1,000 or so operations have an infection develop in the first month. We let patients know the signs of infection that they should look for. When they call us promptly about such symptoms, we are very successful at treating infection without bad results. In an infection, the eye has pain, a big increase in redness, a sticky discharge on the lids (pus), and vision often is much worse. Any two or three of these should lead to a fast phone call to the doctor, even on Saturday night.
Late infection can happen with trabeculectomy and to a lesser extent with tube-shunt surgery even months to years after surgery. Why this is true makes sense if you visualize the operation: it’s a new channel through the eye wall from the inside chamber, then under the flap, and finally under the conjunctiva. If bacteria can get through the first layer of conjunctiva, they can swim or drift inside the eye much easier than in a normal eye, where the white sclera is intact. It’s obviously still hard for bacteria to get in, because among thousands of trabeculectomies, there are few infections. The rate is about one in one thousand operations each year after surgery. Again, one key to minimizing the risk of infection is to have patients recognize symptoms of infection and call in quickly. A bleb with an overt leak in the conjunctiva makes infection even easier.
For about a year after any surgery on any body part, the nerves in the area have to regrow and during that time things feel different. Most often this is minor and can be soothed by taking artificial tear drops (over the counter type). Many patients describe this as “it doesn’t quite feel like my old eye yet”. It is very uncommon for us to have to do surgery to fix these feelings, although occasionally the bleb gets too high or extends too far down all around the white of the eye and needs to be revised.
There are those for whom trabeculectomy works better and those in whom it’s unlikely to win. The success rate is higher in eyes without past surgery and in older persons. It’s like a senior discount: older persons heal worse, so the surgery works better. It's not so favorable if you scar a lot, have had other past eye surgery, or have ongoing inflammation in the eye or some form of secondary glaucoma.
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.