 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
Take Home Points
There is presently no cure
Successful treatment can stop meaningful vision loss
Nerve cell replacement research has taken initial steps
When she was 90 years old, Dr. Quigley’s wonderful Grandma Mamie told him she was having trouble putting on pullover sweaters because her shoulders had arthritis. “Harry,” she asked, “you’re at that medical school Johns Hopkins, when is my shoulder going to get better?” He had to help her understand that we weren’t going to cure her shoulder, but we could buy her button-up sweaters. An important part of helping persons with glaucoma is to channel that hopefulness that Mamie expressed into flexibility to deal with what they’ve got. (Mamie kept winning at Bingo and playing bridge for some time afterward).
In this section, we’ll discuss two forms of definitive treatment for glaucoma, one may happen in the future, and one is what we can do now. The future hope is to restore vision that has been lost. That can’t presently be done. The present treatments can slow the process so much that no meaningful loss occurs in the person’s lifetime. Successful glaucoma surgery can lower eye pressure to a safe level (see section on Operations for glaucoma). Such surgery can last for many years without need for any eye drops or medicines. But, since there are some eyes after surgery that start needing medicine or more surgery again later, it is important to keep having doctor’s exams regularly even when successful surgery has been done. Remember, glaucoma is a chronic condition, so routine checkups will be needed throughout a person’s life, just as they are for other serious illnesses where a remission has been produced, to be sure it doesn’t come back. For now, we have several ways to lower eye pressure to really slow vision loss from glaucoma.
The successful treatment for most persons with glaucoma is to take daily eye drops indefinitely. Several laboratories and companies are presently working on a variety of ways that the medicine for glaucoma could be given only every 3 months, and ideally only once per year. These approaches will probably include placing the medicine as a deposit under the surface of the eye or even inside the eye in the doctor’s office under sterile conditions. This may sound scary, but for another eye disease called age-related macular degeneration, inside the eye injections every month are already proving to be a sight restoring method. Sustained delivery methods could really increase the number of those with glaucoma who no longer need to take eye drops every day.
There are several things that could be placed on or in the eye that could help. Some would be drugs in a long-lasting formula that lower eye pressure. Others would be carriers made from modified biologic particles that get inside the eye cells in the front or back of the eye. Once inside, these biologic carriers fool the cells into thinking that the DNA they carry should be translated like a normal gene and the substance that is produced is made by the cell as if it were a natural molecule. The Glaucoma Center of Excellence team has already tested several such molecules that slow glaucoma damage in animal models of glaucoma. Ideally, one injection of such a biologic carrier would last for years to protect the eye. This may sound like Star Wars, but one eye disease called Leber’s Congenital Amaurosis has already been helped dramatically in human eyes by this type of approach. People with that disease have the fortunate situation that when the biologic carrier was injected, they actually saw better. This insertion of DNA is called gene therapy, and there are active research programs to use this approach for glaucoma.
Gene therapy is only one of the things now being included in the approach called neuroprotection research for glaucoma. This type of treatment, when it becomes available, will involve any method that keeps nerve cells alive longer—and preserves the vision that the person has at that time. But, gene therapy and neuroprotection will not restore lost vision. In general, these methods do not try to lower eye pressure, but rather they make the eye or the nerve cells less likely to suffer from the effects of eye pressure and the other negative things that glaucoma does. We now have more than a dozen types of potential neuroprotective drugs that have been shown to work in this way in mice, rats, and even monkeys. One full trial of a drug called Memantine in over 1,000 patients was conducted to see if the pill would slow the rate of visual loss in glaucoma patients. The drug didn’t work well enough to be recommended for patients with glaucoma. When we talk to glaucoma patients and their families, there is often a wonderful hopefulness that adding some treatment to the standard approaches will be helpful. Consideration of the things that are called “alternative therapies” is given in section Are there treatments other than lowering eye pressure?
Standard glaucoma treatment has been shown to slow the progress of the disease in the majority of patients to such an extent that they never become more impaired than they are at the time they discover they have the disease. That isn’t a cure, but it is a comfort. But, for those who have very significant vision loss from glaucoma, the hope is that we will find a way to restore vision. For some eye problems, there are actual improvements to be expected from treatment. Cataract means that the lens inside the eye has become clouded. Surgery is commonly done to remove the foggy lens and replace it with an artificial one. Cataract surgery routinely restores normal vision to those for whom cataract was their only problem. Yet, in glaucoma, the loss of vision is due to death of the nerve cells called ganglion cells. These cells do not replace themselves as our skin cells do, for example.
So, to be able to restore vision, we must put back a lot of nerve cells. And, they can’t just be thrown into the retina, they have to go in the places where previous ones lived. And, they have to link up on one end with the other retinal nerve cells they normally get information from, as well as to grow a fiber along those 2 inches up to the brain and link up with the partner cells in the next relay station. And, the connections (synapses) need to be made in a way that produces useful vision images, without messing up the existing connections for the parts of vision that haven’t been lost from glaucoma already.
As you can see, that’s a lot of “And’s.” But, 10 years ago, we held a meeting of scientists in which all the group talked about was how impossible it would ever be to restore vision in glaucoma. Dr. Quigley‘s lab and other research groups went to work and since then we’ve accomplished some of the initial steps. First, we know where we can get the nerve cells that we need, they can be produced from stem cells that are available in laboratories (Figure 9).
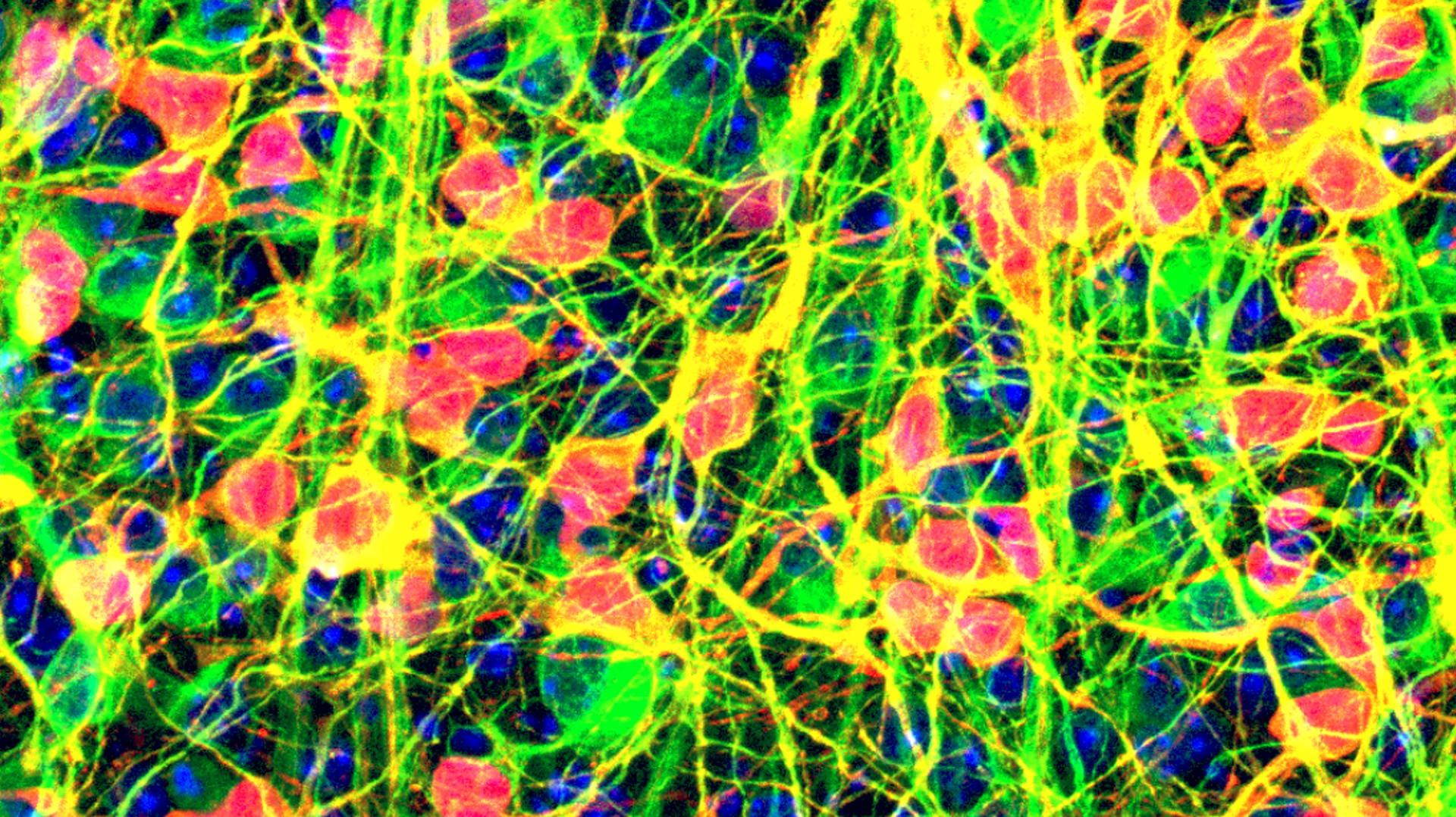 |
Scientists call something a stem cell when it can turn into many different things, like a bone cell, an ear cell, or a heart muscle cell. Stem cells are present in fetuses at an early stage after fertilization and we have learned a lot about development from them. Clinician-scientists from the Glaucoma Center of Excellence have turned such stem cells into the nerve cells we need to replace vision in glaucoma, the ganglion cell. They are now working in lab experiments to take the steps needed to teach them to incorporate into the eye in a functional way. Other “stem cells” have been produced by treating adult cells in special ways. These have the advantage that if we started with your cells (like from skin) they might be less likely to be rejected as foreign tissue.
Progenitor cells from the eye and from some other tissues (like the bone marrow where blood cells start) have been tested as replacements in the eye and there are some positive results. Progenitor cells have been convinced to move into the retina of animal eyes and have lived there for brief periods. No one has yet succeeded in finding a way to take the next steps: getting the synapse connections wired up to the existing cells in the retina and growing a fiber up to the brain. We have plans that hopefully will beat those problems. But, more work is needed and no therapy will be available for a number of years.
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.