 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
Take Home Points
Measuring eye pressure (tonometry)
See if angle is open or closed (gonioscopy)
Test side vision (visual field test or perimetry)
Examine optic nerve head (ophthalmoscopy, photography, imaging devices)
So, if persons with glaucoma rarely find it themselves by noticing something wrong with their eyes, how does an eye doctor find it? The answer is through careful examining and good detective work. First, we look for those contributing risk factors that make it more likely that you might have either open angle or angle closure glaucoma. If you have two or three of these risk factors (such as having a blood relative with it or being an older African American who is near-sighted), it’s mandatory to do the detailed exams for glaucoma that we’ll discuss here. Why not just do all the tests on everyone? In every eye exam, the doctor asks questions about risk factors (called taking a history). The doctor also measures your eye pressure and looks into the eye at the optic nerve. But, it is a waste of time and money to perform all the other tests on everyone, because many people are at very low risk of glaucoma.
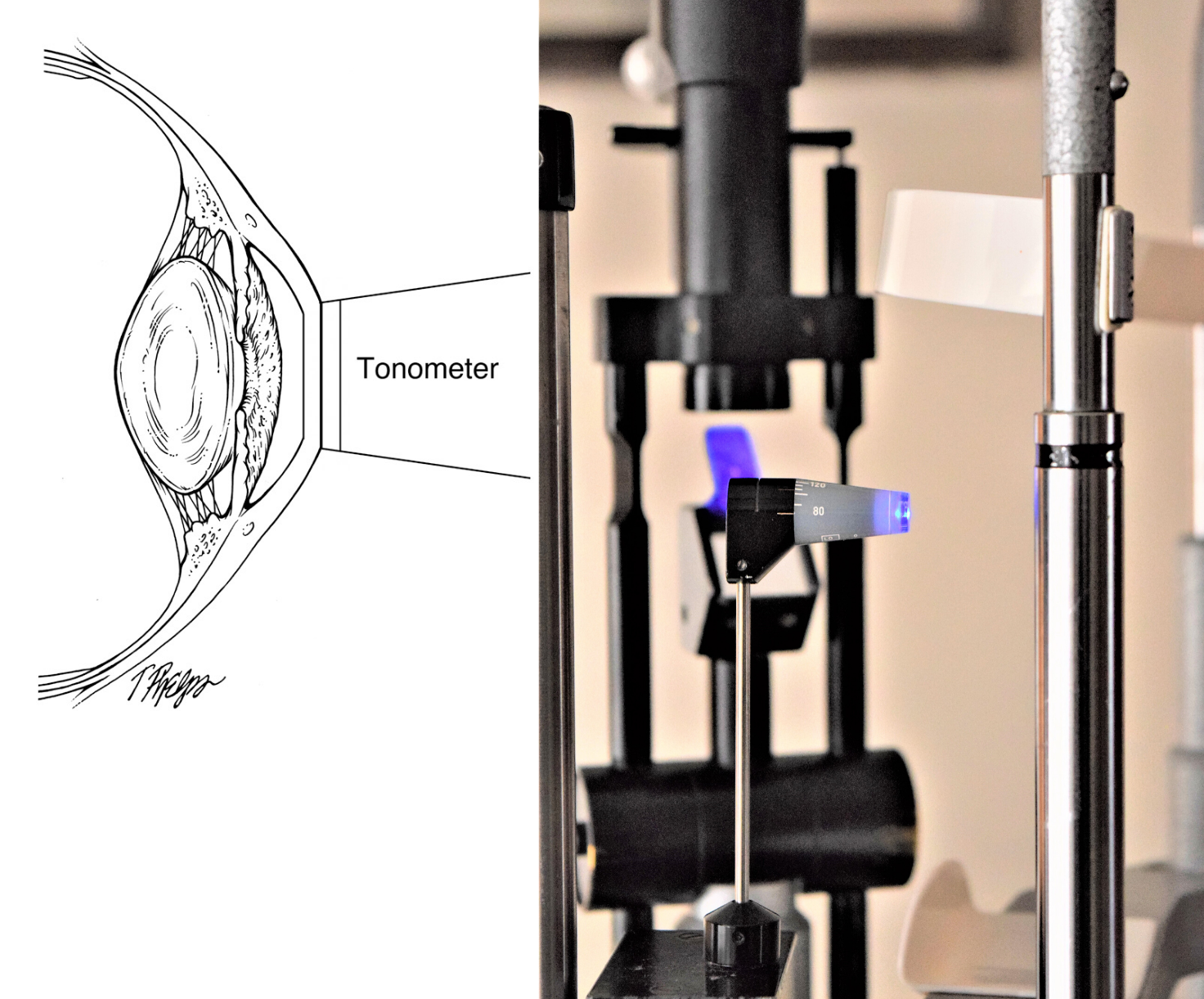
Eye pressure measurement is most often done with a tool called a tonometer (Figure 10). There are several methods to do tonometry. The one that is used most now was invented by Hans Goldmann, a Swiss eye doctor who invented many other important diagnosis tools for glaucoma. This instrument is part of the big machine that is attached to a chin rest device that slides up in front of the patient with a pair of binoculars for the doctor to see things magnified and with a bright blue light. After numbing the eye with eye drop anesthesia, the Goldmann tonometer presses against the eye. The force with which the eye pushes back is used to estimate the pressure inside the eye. The tonometer is highly accurate and is the “gold standard” for glaucoma. Patients should not hold their breath during measurement because it can falsely elevate your eye pressure (you can slowly breathe through your nose). For most patients, the eyelids have to be held out of the way with the doctor’s (or technician’s) fingers or they will make the measurement impossible—or worse, they can artificially raise the measured pressure by pushing on the eye.
Some eye doctors use something called “air puff tonometry” instead of the Goldmann tonometry method described above. The air puff is not as accurate but can be used as a screening tool. Other ways to measure the eye pressure that are not routinely done any longer will be briefly mentioned here: Pneumotonometry involves using a diaphragm connected to a gas filled chamber to measure the eye pressure, and in Schiotz tonometry, the indentation of the cornea by an object of known weight gives an estimation of eye pressure.
 |
Tonometry is usually easy to go through, since the eye has been numbed by drops, so you feel nothing. During the actual measurement, the instrument can rub some cells from the cornea if it is not done gently. If the patient rubs his or her eye during the 20 minutes afterward, the cornea can also be scratched. This rarely happens, but can cause substantial pain or a feeling like something is in the eye. The doctor should be made aware if this happens.
Pressure was originally measured using the change in a column of mercury that we now only see in temperature thermometers. Although the instruments have changed, the unit of measurement for pressure is still the same, and the range of normal eye pressure is from about 10 to 20 in units of millimeters of mercury. But, pressure measuring doesn’t tell us who has glaucoma very often. Those who have open angle glaucoma only have a pressure outside the normal range half the time. The other half of those with pressures higher than normal doesn’t have glaucoma (and may never develop it). So, having a higher than normal pressure is a contributing risk factor, and should lead to a full detailed glaucoma evaluation, but it isn’t glaucoma. Those with angle closure glaucoma more often have higher than normal pressure, but not always.
Eye pressure varies a bit during an average day and from day to day. It can range 10 millimeters of mercury up and down in those with untreated glaucoma. It is, on average, higher first thing in the morning and lower in the evening, though this is not true of every person. It is higher when we are lying down than when we are standing (mostly this relates to how high our eye is compared to our heart). Hanging upside down or doing headstands, for example, causes eye pressure to go much higher (see section How should you change your life?). There is some evidence that greater variation in eye pressure may be worse for glaucoma patients. Some doctors advocate trying to estimate the degree of variability by measuring patients more often, on different days, at different times of day, or throughout one whole long day of measuring (called diurnal measurement).
Recently, newer tonometers were invented to solve problems that come up with pressure measuring. First, the Goldmann tonometer is hard to use when the cornea (the clear front of the eye) isn’t normal in shape. Second, we’ve known for a long time that the pressure reads differently depending on how thick the cornea is, called central corneal thickness or CCT. This is measured with a small instrument called a pachymeter. The normal cornea is as thick as 5 pages of a book stacked together (about half a millimeter), and the tonometer depends on the cornea being that thick to be accurate. If your cornea is half a page thicker or thinner than the average, eye pressure will read differently. Thinner corneas read too low and thicker ones read too high. Persons with thinner corneas have been shown to be more likely to develop open angle glaucoma when they start out as suspects (see section How did you get glaucoma?). While several new instruments have been designed, they all have issues that keep them from being perfect enough to avoid these problems. The new instruments have disadvantages of their own (like being much more expensive to use). Of course, the doctor and patient want to have the best reading on what eye pressure is, so accurate tonometry is important. But, it is even more important to know how much the pressure has been changed from before therapy to afterward (see section What is the target eye pressure?). That is much less dependent on having the exact true eye pressure and more dependent on having lots of pressure measurements.
One new tonometer, the iCare, has solved some problems well. It can measure pressure without putting in anesthetic drops, so for patients who are allergic to those drops we can now get a good reading. Equally important, we can get good pressures in infants and children much more often with this tonometer. That means fewer times when a child must be put under anesthesia to find out what their pressure is (see section Children and glaucoma).
 |
Take Home Points on Tonometry
Applanation measurement is the present gold standard
Having “normal” pressure doesn’t mean you don’t have glaucoma
Having higher pressure doesn’t mean you do have glaucoma
Eye pressure varies through the day and night, more in those with glaucoma
Thickness of the cornea affects pressure measurement
There is a new tonometer that doesn’t need eye drop anesthesia
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.