 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
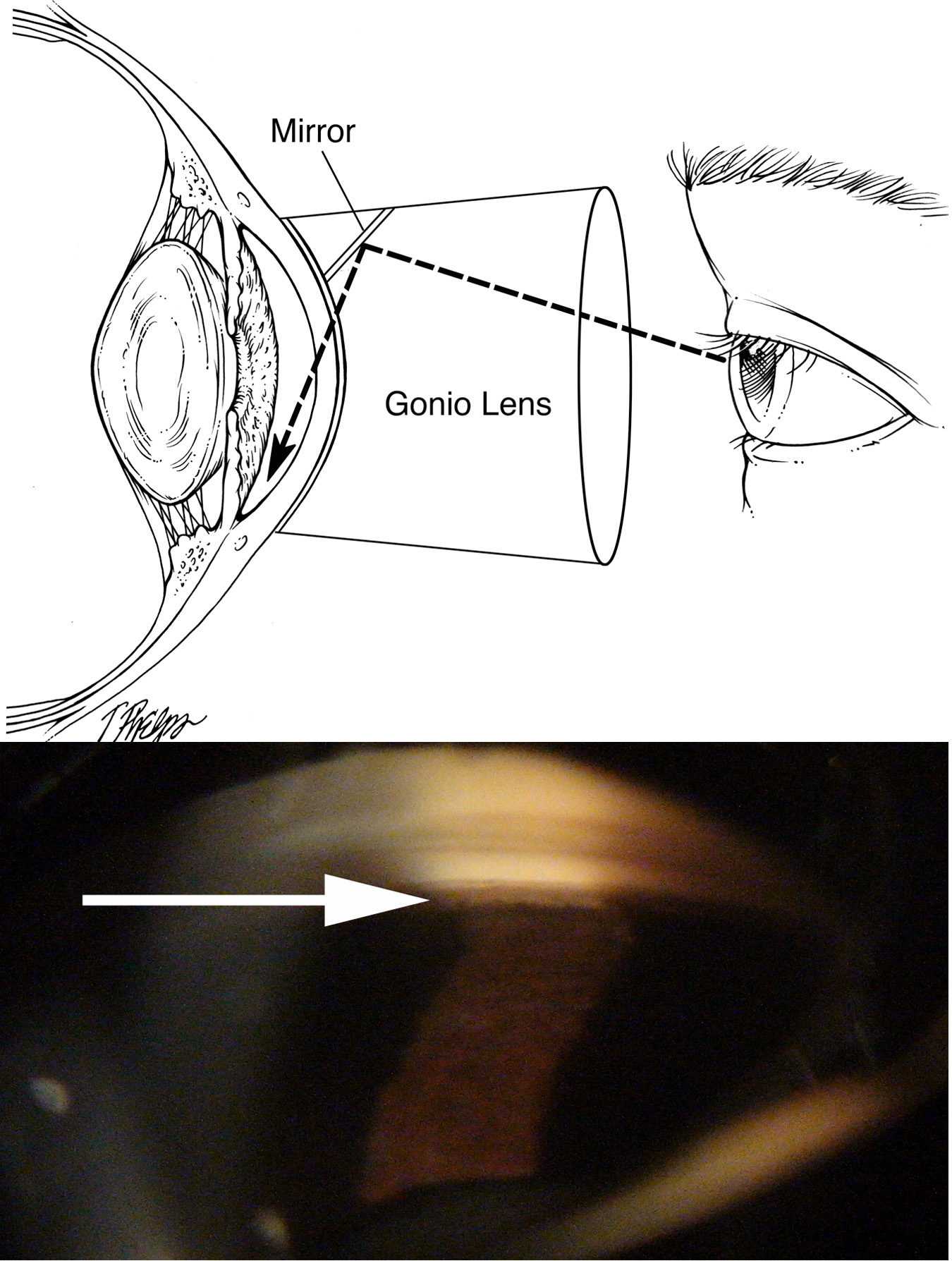
The second test done for all glaucoma patients is to look at the angle, where aqueous humor leaves the eye (Figure 12). Because the angle is inside the eye, essentially around a corner on the interior, it needs to be seen with a big contact lens prism called a gonioscope. There are several types of gonioscopes, but all are placed against the eye after it is numbed and have mirrors to allow the doctor to see several things. First, is the angle open, closed or somewhere in between? The angle runs all around the eye in a circle, so all 4 zones (up, down, nose side, temple side) must be looked at by turning the gonioscope (or having one with 4 mirrors). Second, doctors look for places where the iris has permanently stuck to the meshwork. These are signs of past, significant angle closure. Third, we look for other signs of abnormality, like new blood vessels or torn places from past injury (see section Secondary glaucoma).
 |
Unfortunately, eye doctors don’t always do gonioscopy when it is appropriate, as our researchers found when we studied the charts of glaucoma patients from across the United States. Almost half of these charts did not have any documentation that the doctor had done gonioscopy or knew if the angle was open or closed. Patients who are glaucoma suspects or who have glaucoma will want to ask their doctor what their gonioscopy shows.
Gonioscopy is the main test that tells whether angle closure is likely. It isn’t an all or nothing decision, and no eye doctor can classify every angle for certain. In probably more than 95% of all eyes, we could get 3 eye doctors to agree about whether an angle is open or closed. But, it is in the few in-betweeners that we must use judgment and make a joint decision with the patient about the best course. The decision in the case of angle closure is whether to make a laser hole in the iris immediately or to wait and watch to see how the eye does without laser iridotomy. Detailed discussion of this issue is in the section Why isn’t glaucoma either there or not there? - What makes you an angle closure suspect?
For some years, glaucoma centers like the Wilmer Institute have added newer exam methods to evaluate the angle to their gonioscopy. The most recent and promising of these is called anterior segment optical coherence tomography, or AS-OCT (Figure 6). It is a painless imaging test that requires no anesthesia and has a dim light that reflects from the eye and makes a picture of the cross-section of the angle along with the cornea and iris. Our research with this technique has shown that the iris acts differently in those with angle closure—it is less “spongy” is one way to describe it. We and others are now looking for ways to show scientifically that using the new imaging methods will tell us much more about who needs a laser iris hole and who does not.
Take Home Points on Gonioscopy
The doctor should evaluate the angle in possible glaucoma patients
Most often the angle is open
Angles that are narrow may need to have a laser iris hole made
Gonioscopy is not always certain to give the answer and newer methods are in development
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.