 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
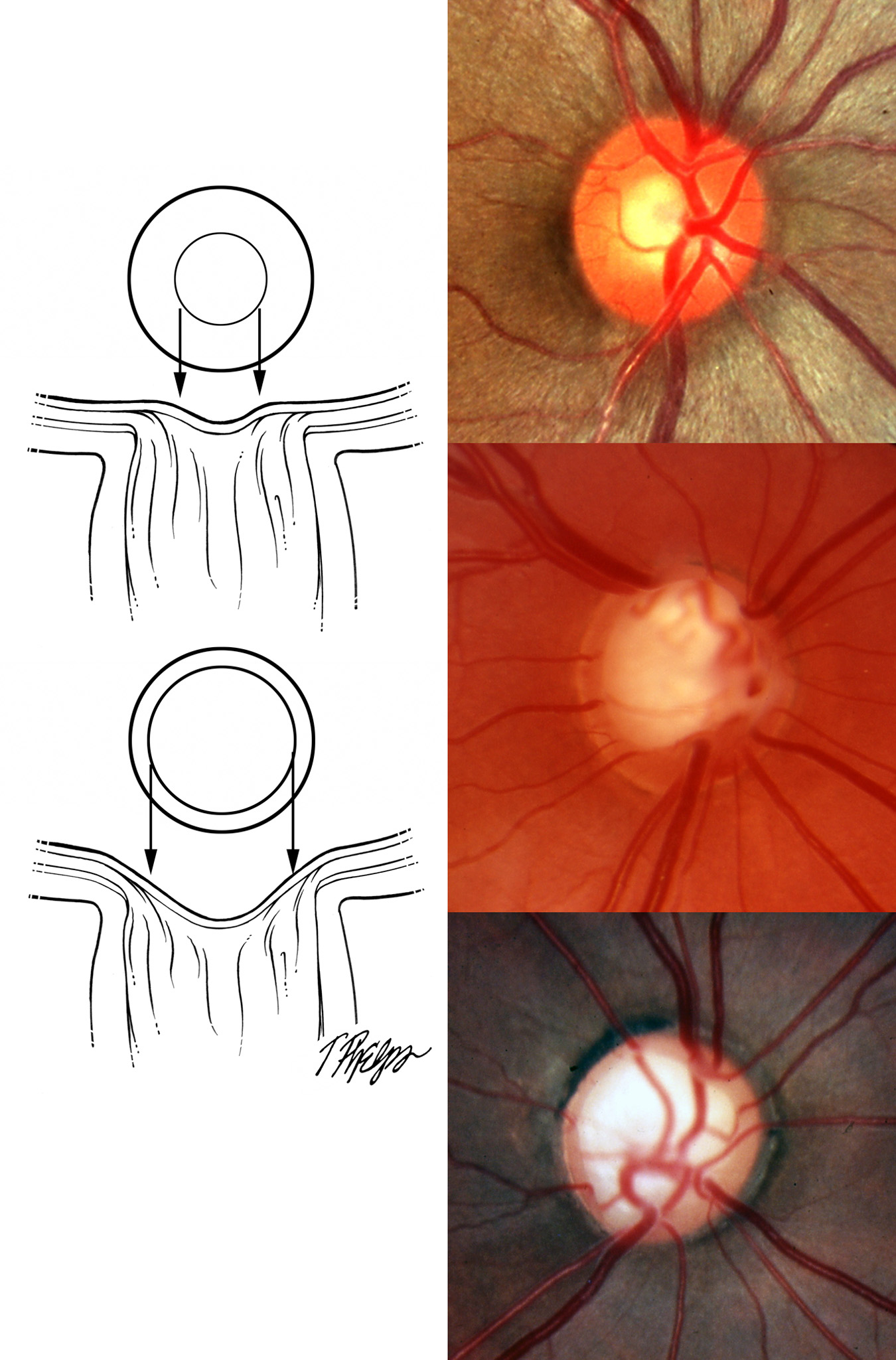
The third important exam method used to identify glaucoma is looking at the retina and optic nerve head for signs of glaucoma damage. In this exam, called ophthalmoscopy, doctors look for signs that structural loss of ganglion cells and their fibers has already happened. Ganglion cells are scattered all over the retina, and their fibers converge on the optic nerve head like roads coming into a big city. The layer of fibers gets quite thick just at the nerve head and as the fibers pile up and dive into the opening. The nerve head, often called the disc, is mostly filled with fibers. There is left over space in the middle of the nerve head called the cup, and the fibers are grouped around the cup in the rim. We all want to have lots of fibers, so we want a big rim (and by subtraction, a small cup). When we compare the size of the cup to the size of the whole disc, we talk about a “cup to disc ratio” (Figure 13). The bigger the ratio, the more empty space there is in the nerve head. That space may be left behind when nerve cells die. The average cup to disc ratio is about 0.4, and ratios of 0.7 or greater happen only 2.5% of the time, so cups this big raise our suspicion that glaucoma might already have started (Figure 13).
 |
This test should be performed at least once per year in those suspected of having glaucoma and even more often in those with established glaucoma. Patients who are having ophthalmoscopy often have the pupil dilated with drops for the exam to allow a better view and to let the doctor get a stereoscopic (two-eyed) image to see the optic nerve head in 3 dimensions. In some patients, it is possible to see the optic nerve head well without dilation. When it is necessary to use drops to dilate the pupil for this exam, the person may be more sensitive to light for a couple of hours and for those who still can read without reading glasses, their near vision is poor for a while due to the drops. The examining light is very bright, and while it is not dangerous, the person often can’t see well for a few minutes after the exam. This is like staring at a car headlight and looking away; right afterward one sees only blobs of color that block our vision.
Glaucoma causes loss of fibers in groups that run together, so in looking at the nerve head, there is sometimes a tell-tale notch or local loss of fibers in one area of the rim, typically at the top or bottom (see Figure 13 and Figure 14). Big differences between the two eyes in the size of the cup are also a way to identify glaucoma that has started in the eye with the bigger cup. And, occasionally, bleeding in little splinter-like streaks happens on the nerve head to indicate that glaucoma is active.
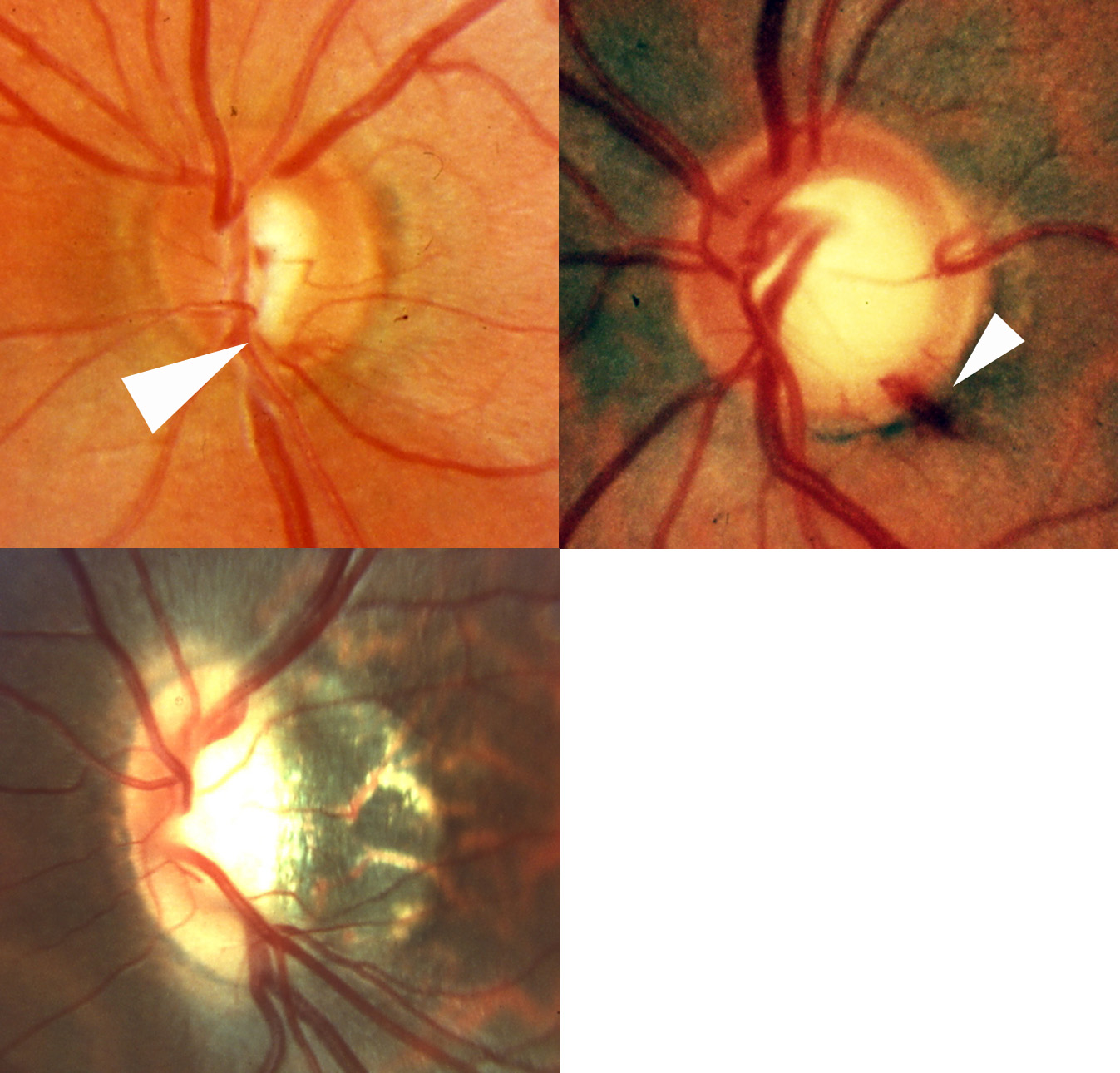 |
If the changes in the nerve head by ophthalmoscopy identify glaucoma, then why are some cases not diagnosed early enough? Perhaps the biggest problem is that the structure of the nerve head varies a lot among people. Many human features have a wide normal range. There are short people, 5 feet tall, and 7 footers, so just being outside the “normal” range doesn’t mean that a disease is present. The cup can be big in some discs just because the disc itself is big and there’s lots of left over space after the fibers go through. That leads to over-diagnosis of glaucoma in persons with big discs. Small discs that start with no cup space can have real damage when the cup to disc ratio is in the middle of the average normal range. And, some discs have a tilted or distorted shape (Figure 14, bottom left) that makes judging the cup to disc ratio very hard, even though the eye sees just fine. Having a disc size or shape that is different from normal isn’t a disease in and of itself and does not predispose a person to having glaucoma. However, it may make a person’s nerve seem more suspicious and therefore require more careful monitoring than someone with a disc that is of normal size and shape. There is some influence of race in disc size, for example, African-derived persons on average have larger discs.
To add information during ophthalmoscopy, eye doctors started looking just outside the nerve head at the layer of nerve fibers as they came toward the disc to see if they were missing. This helps quite a lot with the unusual shaped discs to tell if there is fiber loss. But, this nerve fiber layer exam itself has variations and is harder in persons with light pigmentation than in darker individuals. The Wilmer Glaucoma Center of Excellence did a landmark study that showed one could predict functional glaucoma damage 5 years earlier by doing this nerve fiber layer exam.
For many years, it was most common to record how the nerve head looked by taking color photographs (as in Figure 13 and Figure 14), often doing pairs of them to allow a stereoscopic view. These were repeated at intervals and the appearance of the nerve head as the doctor looked at it in the office was compared to previously taken photographs to see if the eyes were the same or had gotten worse. Color film gave way to digital photographs during the last decade in these cameras. But, these photographs needed to be taken with very bright flashes of light and with dilated pupils. The patient’s vision is quite dimmed for a few minutes after this procedure and it is hard to drive home or see to read for some time afterward. There is still some role for this type of photography.
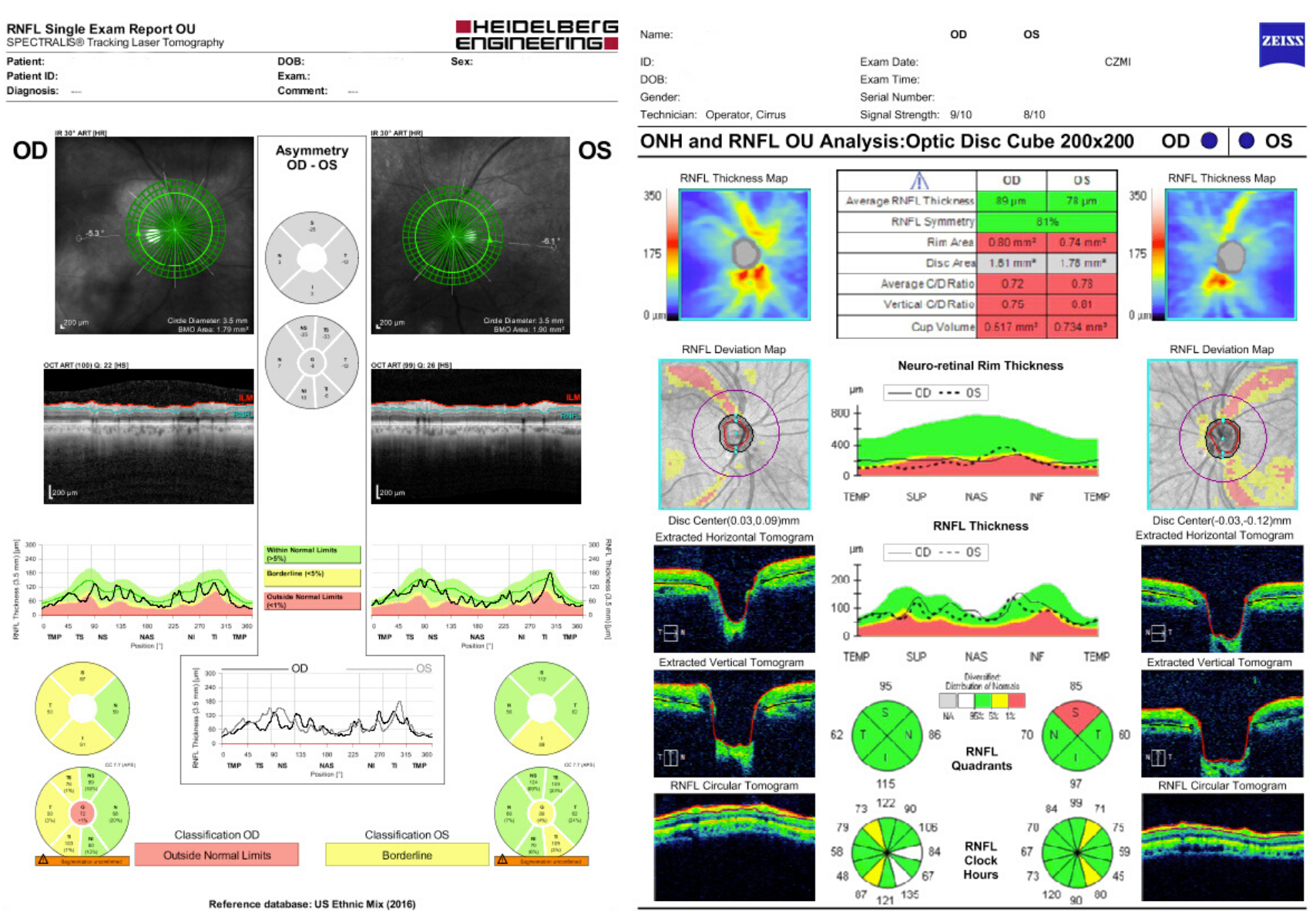
Both the need to have quantifiable information and the lack of convenience of color photographs has stimulated the development of digital imaging methods to assess glaucoma progress and stability. We now can measure the thickness of the nerve fibers with several such instruments, more comfortably and with greater ability to measure for change. Some of these instruments concentrate on the topography of the nerve head—kind of like measuring the slope in and out of a volcano’s cone (Figure 15). Other instruments are good at estimating the number of nerve fibers and ganglion cells by making an optical thickness measurement (Figure 15). The true strength of these instruments has not been fully achieved yet, as their sensitivity is still being improved. The maximum help they give will be realized when we can depend on them to tell us if an eye’s fibers have decreased quantitatively. That is an important measure of whether the patient is doing well (staying the same) or getting worse (losing fibers). There is considerable research being done to see which instruments allow us to judge how patients are doing. Artificial intelligence methods may soon assist the experienced eye doctor to interpret these tests.
 |
Take Home Points for Ophthalmoscopy
Doctors look at the optic nerve head to judge whether loss of fibers has happened
Glaucoma causes differences between right/left nerves, local fiber loss and tiny blood spots
Variation among persons in nerve head appearance must be taken into account
Nerve fiber layer loss seen both by the doctor and with instruments can improve diagnosis
Change in optic nerve head appearance over time can be important
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.