 | Glaucoma: What Every Patient Should Know |  |
|---|---|---|
| Previous Section | Next Section |
Take Home Points
Acute crisis is a true emergency and needs attention immediately
You or your doctor may have caused the crisis by doing something to dilate the pupil
Symptoms: eye pain (headache), bad vision in one eye or halo vision, red eye, pupils of different sizes, nausea
Immediate treatment is to make a laser iris hole (iridotomy in both eyes)
Some are cured forever, but others need continued treatment after laser iridotomy
Two special conditions need particular therapy: plateau iris syndrome, malignant glaucoma
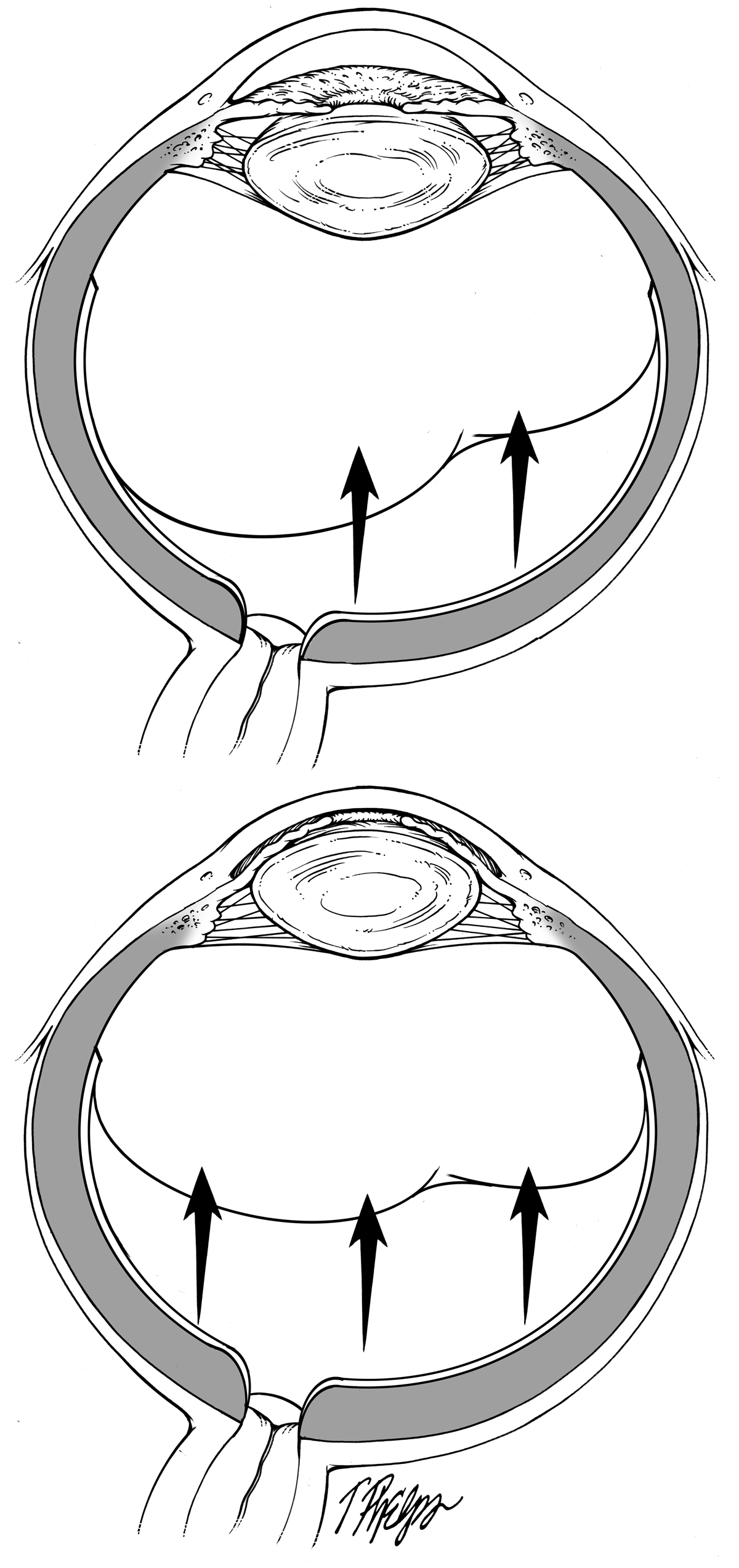
Acute angle closure crisis deserves its own special mention, as it is one of the few true emergencies in the glaucoma world. Of all of the forms of glaucoma, angle closure has a much greater chance to cause permanent vision loss than open angle glaucoma, and the acute crisis (frequently called an acute attack) probably accounts for a lot of this damage. The mechanism by which it happens was described in the preceding section (Why isn’t glaucoma either there or not there? - What makes you an angle closure suspect?). It happens to those with angle closure under the situation where aqueous humor movement from behind to in front of the iris is so blocked that the pressure behind the iris pushes it against the meshwork and stops all aqueous outflow (Figure 7). Eye pressure can rise to numbers like 70 millimeters of mercury (compared to the normal 15). This is so high that permanent damage to ganglion cells in the optic nerve happens in days to weeks rather than the much longer, slower process of typical glaucoma.
It is the sudden increase in pressure that causes the severe symptoms of the attack. A link between the stomach and the eye causes an attack to be not only the worst pain that people ever remember having, but also it causes nausea and vomiting. Sometimes the stomach problem is so prominent that people go to an emergency room and the staff pays attention to that, thinking it is appendicitis, before realizing that the eye is the cause. Acute attacks also get misdiagnosed as migraine headaches.
The eye symptoms of acute crisis are pain, poor vision or halo vision in the involved eye, redness of the white part, and a bigger and irregular pupil shape. More than 90% of acute crises are in one eye only, but for one in 10 persons it happens in both eyes. In order to see if an eye problem is in one eye or the other, one should cover with the hand on one side then the other. In the excitement of being in pain, we often forget to do such simple things.
The things that can set off the crisis are those that can cause the pupil to move to the danger position, half-way dilated. These include stress and excitement, spending time in a dark place (such as a dimly lit restaurant), and being exposed to medications that dilate the pupil a bit. This happens during general anesthesia for surgery, since a drug that dilates the pupil (atropine) is given by anesthesiologists. If you have bad eye pain after surgery under general anesthesia, have an exam by an eye doctor immediately. Acute attacks can also be caused by the many pills that are given that can dilate the pupil while helping you with things like urinary incontinence, sinus troubles, and upper respiratory colds. The Food and Drug Administration doesn’t distinguish the various kinds of glaucoma in its warnings on drugs about “glaucoma”, so if you are an angle closure suspect who has not had iridotomy, call your eye doctor before taking any of these drugs. Most of the time, you’ll hear that it’s fine to take them. After you have an iridotomy, you can take any of these drugs safely. The final types of drugs that can cause acute crisis are those used in the eye doctor’s office to dilate the pupil for examination of the inside of the eye. We’ve seen this a number of times over the years, and patients who have had dilating drops and have pain the night of the exam and especially into the next morning should go right back immediately to be checked. There are a group of medicines that can cause a very unusual form of acute angle closure in people who otherwise weren’t at risk for it (they don’t have small eyes or other risk factors for angle closure). One such drug is topiramate, a headache pill which is also used in epilepsy. Another group of drugs that can do this are some antibiotics (see section Can the treatments be worse than the disease?).
If you think you are having an acute angle closure crisis, go to the office of an ophthalmologist (a medical doctor who does surgery and laser surgery) or to an emergency room that you are sure has an ophthalmologist on call to come there and see you. Most metropolitan areas have an “eye trauma” center designated where immediate, appropriate care would be available. Don’t drive yourself there, get a ride or take a cab.
The immediate treatment for acute crisis will most often fix it in the first hour. The pressure is lowered by either eyedrops or by letting a small amount of aqueous out of the eye with a tiny needle. This sounds gruesome, but you’ll be numbed with eye drops, so you won’t feel it and it immediately relieves the pain. Sometimes, in order to begin the lowering of pressure, a laser is used to treat the outer part of the iris to move it away from the meshwork to let aqueous out faster (laser iridoplasty). The vast majority of crises are relieved as soon as a hole is placed in the iris with a laser (Figure 18). This instrument, called a neodymium-YAG laser, can be focused inside the eye to make the iris hole, without making any incision or hole in the eye wall (cornea). There is a slight feeling of pressure and a flick, but typically only eye drop anesthesia is needed. Several deliveries of the laser may be needed to make a hole about 0.5 millimeters in diameter. That’s all it takes to relieve most crises. Occasionally, a second type of laser is used in very thick irises (called a continuous wave laser or diode) to thin things down before penetrating with the neodymium-YAG. High quality centers have both available to use. The opening is usually small enough that others can’t see it from normal social distances. Those who get within 6 inches of your face for long enough to find the iris hole are people who know you well enough that they’re concentrating on other things. Sometimes a small hole is made initially, and it is made bigger a month later.
The other eye should have a hole made, too, though most persons want to wait a day or so to try to get back vision in the first eye. Putting it off for a long time is a really bad idea.
If the crisis has been going on for longer than a day (and you may not have been aware of it during that time) or if there have been preceding little attacks in the past that led up to this one, the laser iridotomy alone is not going to cure everything. There can be scars in the angle that won’t go away, leading eye pressure to stay high. There may already be damage to optic nerve structure and visual field function, so that vision is never fully normal again. Haziness in the lens of the eye (cataract) may be already present or develop quite quickly after the iridotomy due to the prior high pressure.
Some have suggested that removing the lens (cataract surgery) would be a good treatment for acute crisis. Since the reason for the crisis is severe blockage of fluid movement between the iris and lens, that is a correct statement, but removing the lens and replacing it with an artificial intraocular lens by surgery in the middle of an acute crisis is very difficult. Only the most experienced cataract surgeons, working at a center with extensive equipment to operate on the retina and vitreous inside the eye should even attempt this. On occasion, the acute crisis is not broken by laser iridotomy and by medication—this then calls for forms of glaucoma surgery (see section Operations for glaucoma).
An uncommon type of glaucoma happens in some eyes that seem to have a typical acute crisis, but do not respond to standard laser iridotomy, with pressure remaining high. The doctor will see some special clues that this condition, called malignant glaucoma has happened. Malignant glaucoma got its name because it was difficult to deal with; it has nothing to do with cancer. It even happens sometimes in persons who are not at risk for typical angle closure. The mechanism involves a collapse forward within the eye of the gel called the vitreous that fills the back two thirds of the eye cavity. The best explanation at present is that the process starts, like typical angle closure, with choroidal expansion, and in these folks the vitreous collapses forward due to pressure behind it. The treatments start with lasers, but then additional types of eye drops, oral and intravenous medication, and often surgery to make a channel through the vitreous gel are needed to cure the problem.
 |
If you would like to support the cost of providing and maintaining this book with a charitable donation of any size, please click here.